Tl;dr: We talk about body weight regulation too simplistically. We need to talk about quality and quantity.
There is a famous joke about physicists and it goes something like this, “Milk production at a dairy farm was low, so the farmer wrote to the local university, asking for help from academia. A multidisciplinary team of professors was assembled, headed by a theoretical physicist, and two weeks of intensive on-site investigation took place. The scholars then returned to the university, notebooks crammed with data, where the task of writing the report was left to the team leader. Shortly thereafter the physicist returned to the farm, saying to the farmer, ‘I have the solution, but it works only in the case of spherical cows in a vacuum’”.
This joke is a humorous way of stating that we use models to simplify complex problems in order to understand them. In nutrition and physiology we do this quite often, especially when it comes to explaining weight loss. While this can get us pretty close to the right answer and our current tools work really well from a pragmatic perspective, there is immense value in fleshing out the deeper, underlying concepts surrounding weight and body fat regulation.
Put on your big boy pants and take your nootropics because this is not going to be the easiest or lightest read of the week. Frankly, the internet suffers from lack of deep thinking, so I refuse to apologize for the length of this one. Let this be an exercise in breaking bad habits of reading “fluff” articles. Time to put that gray matter to work.
Thermodynamics in context
Any discussion about the mass of a system has to first begin with thermodynamics*. We shall being by briefly reviewing the three laws of thermodynamics as a refresher. This also is a refresher for my mind.
- The law of conservation of energy: Energy cannot be created or destroyed in an isolated system.
- The Entropy of any isolated system always increases
- The entropy of a system approaches a constant value as the temperature approaches absolute zero.
As the internet has no peer review to stop bad arguments from being circulated, there are a lot of pedantic arguments stating we can’t treat the body as an isolated system; this is nonsense. You can quite easily model the human body as an isolated system with regard to energy input and output. Anyone who says otherwise has not really done much critical thinking on the subject. I will throw myself under the bus here as I have been sloppy in the past and used that argument. This is life, we learn and get better.
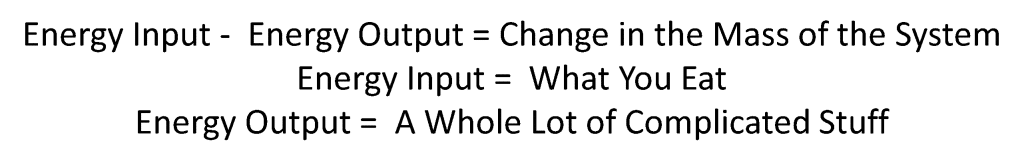
Now, onto context. When we think about thermodynamics and how it applies to the human body we can look at the cellular level and discuss the biochemical reactions and free energy equations, or we can take the pragmatic approach and discuss the notion of overall energy balance. Pragmatism is highly underrated and underutilized, let’s go that route. From the physicists perspective about the spherical cow, we can approximate the changes in the overall mass/weight of by tracking the food that goes in and the energy expended. There have been metabolic chamber studies that measure all of the energy consumed and expended and the change in the energy in versus the energy out and the change in body weight correlate extremely well. There are also tools such as doubly labeled water that can be used to also approximate weight changes to a surprising degree of accuracy.
Now before we proceed any further, let me plant a flag, out in the open for all to see and let you know exactly what my interpretation of the data is on this topic. No matter what your “theory” of weight (or body composition) regulation is, it has to obey the laws of thermodynamics. You simply CANNOT have more energy coming out of the body than going into the body and gain weight, conversely, you CANNOT have more energy going into the body than coming out of the body and lose weight. Thus, any theory one contrives must fall under the laws of thermodynamics.
Calories-in vs Calories-out model (CICO)
One of the current models in nutrition that is equivalent to the physicists sphere is the Calories-in-calories-out (I will take the liberty of calling it CICO) model of body weight regulation. The calories in calories out (CICO) model holds a lot of truth and can explain a lot of the variation in body weight, yet it is incomplete. I like to compare the CICO model with Newtonian Physics… it is accurate and describes gravity for a majority of cases but it is not complete. We need Einstein’s theories of relativity to describe the enormously large* and fast and we need quantum theory for the incredibly small.
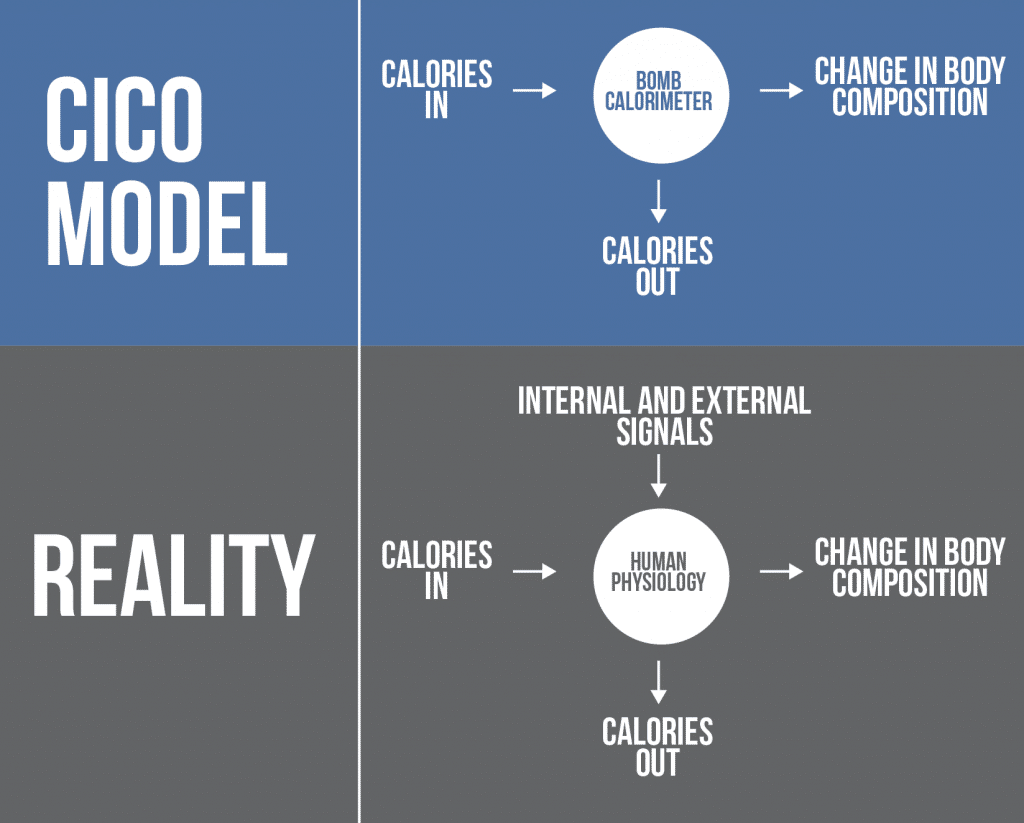
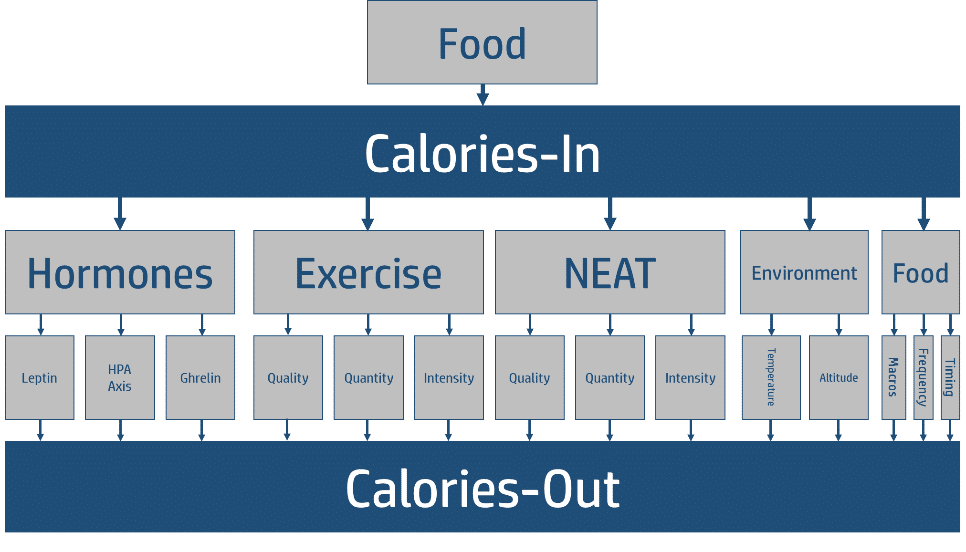
The CICO model is an excellent “first approximation”, but it suffers from what I like to call the “black box” approach where it fails to fully address the nuances of parts of the equation that drastically impact the output. The CICO model treats the body as a bomb calorimeter, failing to account for the complexities of the black box that is human physiology. I offer the following figures to illustrate my point. The second figure is my interpretation of the “physicist’s sphere” where the output is just a complex, indeterminate set of equations
Assumptions
In science we make assumptions. You have to. If you want to accomplish anything meaningful you have to make assumptions. For example, if I wanted to ask a question about some chemical property I have to assume that the atomic theory of matter is correct. I can’t spend 20 years conducting all my own experiments to confirm previous work, I have to rely on assumptions. Good scientists are very forth coming and open about their assumptions. We should do so with regard to the CICO model of weight regulation. Here are the assumptions we make when we adopt a strict CICO model of weight and fat mass regulation (in no particular order)
- When 100% accounted for, the energy into a system minus the energy out should equal the change in the mass of that system (remember E=MC2 shows us that energy and mass are equivalent).
- This model treats the body as a “black box”
- All energy inputs have the same effect on energy outputs
Limitations
Another hallmark of scientific integrity and intellectual honesty is to put forth your limitations in clear detail for all to see. There is no hand-waving, nor is there any pulling the wool over the eyes. So let us put forth the two largest the limitations of the CICO model (I am probably missing a few but these hit the major ones)
- The CICO model fails to account for the differential effects of macronutrients. For example, protein elicits a thermic effect of food and is “harder” to store as body fat than either carbohydrates or fat.
- It completely fails to account for changes in tissue quality. A gain of 5 pounds of lean mass and a loss of 5 pounds of body fat are quantitatively the same in regards to gravity but qualitatively different appearance and health wise (quantitative assessments can also be made of appearance and health)
Hormone Theories of Weight Regulation
On the other side of the weight regulation coin are the hormonal theories. Put simple, these theories indicate that hormones are the primary cause of common obesity and that caloric intake is simple a red herring; it is hormones that are the key. While several hormones have been implicated I think it is safe to say that there are two hormones that deserve the most attention, insulin and leptin, due to their “popularity” and their scientific credentials, respectively (obviously the latter reason holds more weight in a universe that rewards evidence based approaches to problems).
Insulin
Someone smart once said, “I don’t get into debates over certain topics because even engaging in the debate means that there is something to debate. Some sides of some topics just don’t have enough evidence to even warrant a debate”. From my own interpretation of the VAST amounts of data, this is where I stand on the Carbohydrate – Insulin Hypothesis. The vast amount of evidence indicates that insulin is not a primary regulator of body weight. We have covered this topic in depth so I won’t rehash it here. What I will do though is cover the role that insulin DOES play in body weight regulation.
Primarily, insulin functions to regulate blood glucose through hepatic glucose output and peripheral tissue uptake of glucose and coordinate the metabolism of other nutrients (e.g. amino acids and fatty acids). When no glucose is being ingested and insulin levels are low, the liver is “allowed” to produce glucose to keep glucose levels in normal range. When glucose is consumed and insulin is released, the insulin puts the breaks on the liver and then tells the rest of the tissues that glucose and other nutrients are available for uptake and to start using more glucose for fuel. Put simply, insulin is a substrate conductor, it coordinates the metabolism of your different nutrients and regulates levels of these nutrients to sustain life.
Now we need to address the role of insulin in fat storage and nuance the details because they are incredibly important. Insulin does in fact decrease the rate of lipolysis in adipose tissue and does stimulate fatty acid and triacylglycerol synthesis, the science is crystal clear on this. This suggests that insulin is “lipogenic” and promotes overall fat storage and thus obesity. This idea is simple, parsimonious, and honestly quite attractive. This single idea is the impetus behind the carbohydrate-insulin hypothesis of obesity. Unfortunately it misses the mark and when you add in all the information insulin just doesn’t have enough “power” to really make substantial impacts on body fat in common obesity. Let us walk through a few key pieces of data.
The first is that the lipogenic effect of insulin only occurs when insulin has high “action”. Meaning the lipogenic signal of insulin is being heard loud and clear by the cells. In order for insulin to exert “fat gaining” effects it would need to be constantly signaling at above basal levels for high levels of lipogenesis to occur. This is not seen in common obesity for two main reasons:
- In non-diabetic/non-insulin resistant people who become obese have fluctuating periods of insulin signaling with more time during the day with low insulin levels than high insulin levels due to post-prandial insulin rises and low fasting insulin levels (read James Krieger’s series on this phenomena, starting here). When you really look at insulin action over time periods that are congruent with the development of obesity (days, weeks, months, years) you see that the cumulative result of its action doesn’t square with the idea that insulin primarily directs obesity. The next fat storage vs fat burning doesn’t favor the former from this isolated perspective. This becomes even more apparent when we address issue #2 Image c/o www.weightology.net
- As goes obesity so goes insulin resistance. . . . put simple, as body fat rises, body fat tissue (adipose tissue) becomes resistant to insulin, meaning insulin action actually decreases.
- To quote Dr. Stephan Guyenet on this topic, “The fat tissue of obese people doesn’t suppress fatty acid release in response to experimentally elevated insulin or mixed meals as effectively as the fat tissue of a lean individual (18, 19). In fact, obese people release an equal or larger amount of fatty acids from their fat tissue than lean people under basal conditions as well (20, 21). If this is true, then why do they remain obese? It’s simple: the long-term rate of fat entering the fat cells is equal to the rate exiting, or higher. There is no defect in the ability of fat cells to release fat in obesity, the problem is that the fat that is released is not being oxidized (burned) at a rate that exceeds what is coming in from the diet, therefore it all ends up back in the fat tissue.”
- If insulin action were increased in obese individuals due to the elevated insulin than we would observe decreased plasma FA as insulin action promotes lipogenesis and decreases lipolysis in adipose tissue; however we see the opposite in obese individuals. There is substantial experimental evidence to show that as fat mass increases there is an increasing amount of free fatty acids, suggesting fat tissue isn’t really better at storing fat than in lean people. It ends up storing it eventually as more energy is present than needed so eventually it is stored. If insulin action were reducing lipolysis and increasing fatty acid synthesis and storage to the degree that it were the key driver of fat accumulation than this data (below) is very unlikely to be true.
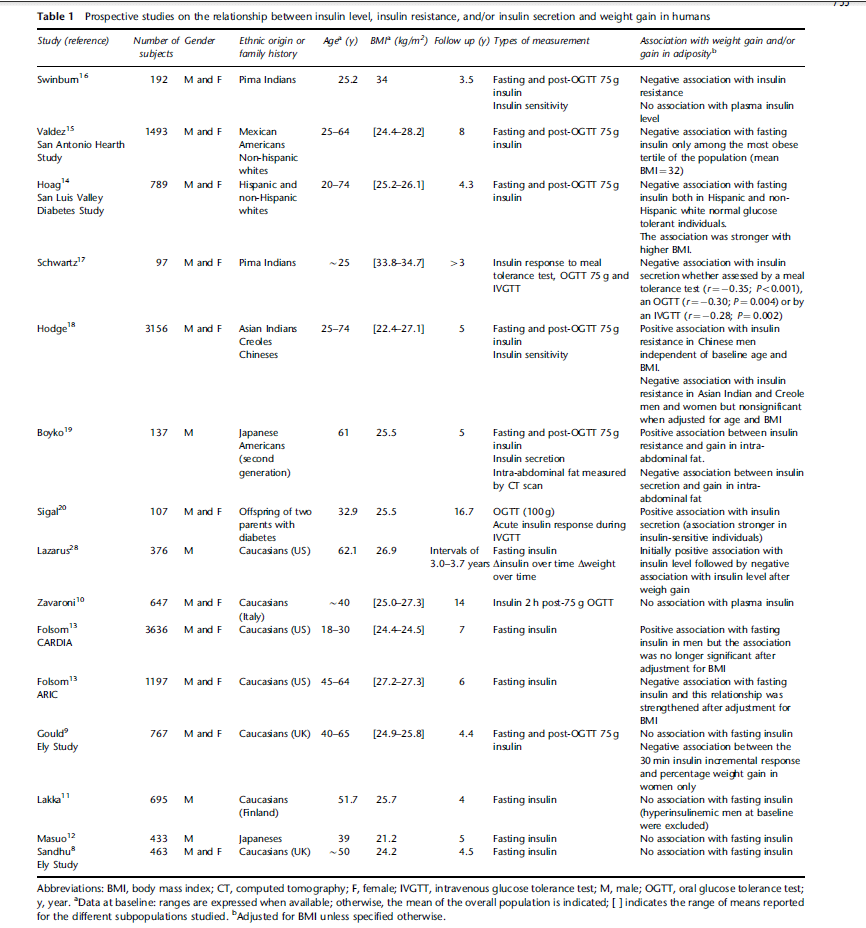
Another key issue point we can make before moving on is that if insulin were indeed a primary driver of common obesity than higher levels of insulin should predict fat gain (remember science is largely about testable predictions). Several studies have looked at whether higher levels of insulin predict future weight gain (see the table below from the review by Hivert et al.). The largely negative nature of this data makes it very difficult to square this data with the notion that insulin, not caloric balance, is a key driver. In fact, I would go as far to say that it plays a very, very, minor role (we will expand on this in later in the post).
Leptin
Leptin is a far better “case study” to examine the role of hormones in regulating body weight, specifically fat mass and the history of leptin is also quite interesting, it involves luck and sewing mice together (parabiosis). The role of leptin is actually fairly multifaceted having both central and peripheral functions. Briefly, leptin works in the hypothalamus through a variety of mechanisms to decrease hunger (mainly through peptide based signaling molecules that regulate both hunger and fullness). Briefly, leptin levels increase as fat mass increases and should result in decreased food intake and increased energy expenditure, bringing the fat mass back down. When fat mass drops too low, food intake increases and energy expenditure decreases until the fat mass returns to a “normal” level. In short, if any hormone should be the candidate for regulating fat mass it would be leptin, not insulin.
In humans who are genetically leptin deficient, they are unable to control body weight and are obese. This obese phenotype is corrected through the administration of exogenous leptin. This demonstrates that leptin can play a major role in body weight regulation when the entire “system” is broken.
Now what happens in people with a complete system, yet have some abnormalities in the system? Is that abnormality enough to really make massive differences in their body weight (i.e. enough to go from obese to lean)? It turns out that in common obesity leptin signaling isn’t “broken” but it isn’t really functioning properly and leptin resistance is often seen. One could posit that you could just administer more leptin and that would fix the issue. It turns out that these clinical trials have been done and leptin therapy doesn’t really correct body weight in any meaningful sense. See here for a very nice, thorough review. The leptin resistance appears to be secondary and resultant from similar biological processes that create insulin resistance (e.g. obesity and inflammation).
So we can use the information we have learned from two hormones that are intimately involved in metabolism, fat storage, and fat mass regulation and come to a few conclusions. Clearly hormones play an essential role in maintaining metabolism. Without insulin you die (typically from diabetic ketoacidosis). Too much insulin you die (hypoglycemia). They also play an essential role in maintaining fat mass. Without leptin you are unable to control fat mass resulting in run-away obesity. However, it appears that in normal, functioning human physiology leptin levels self-regulate through feedback loops to control body fat.
Homeostasis: How the body really functions
The human body is a living, dynamic organism that responds to stimuli; it reacts to a wide range of stimuli: chemical, electrical, and physical. It also follows, albeit roughly, a concept known as homeostasis: the tendency toward a relatively stable equilibrium between interdependent elements, especially as maintained by physiological processes. Essentially it means that when perturbed, the system corrects itself into equilibrium. This equilibrium can be a return to a former state, or a new state that balances out the “forces” being put on the system.
We can use two fairly well known examples to show how robust the human body is and how it adapts quite specifically to a given stimulus.
The first example is the body’s adaptation to exercise stimulus. One simple way to look at this is the differential adaptations to muscle tissue that occur muscle tissue in people who engage in body building style training versus endurance exercise. Body building results in increased muscle protein and increases in muscle cell size. Endurance training increases the mitochondrial density and alters cellular metabolism. Conversely, sedentary behavior results in muscle atrophy and loss of mitochondria and decreases muscle metabolism.
The second example is testosterone. We know that physiological and supraphysiological levels of testosterone can have substantial, divergent effects on muscle tissue. The administration of supraphysiological levels of testosterone is well documented to increased muscle mass while simultaneously decreasing fat mass. Now when you add resistance training on top of testosterone you magnify these effects as you have a chemical stimulus (testosterone) and a physical stimulus (the mechanical tension of weight lifting) working synergistically.
We can continue with examples such as these ad naseum, but I think they illustrate the point. The body is highly dynamic and aggregates a lot of signals into adaptations. As such, both the CICO model and the hormone model are incomplete. They only address one signal, neglecting the others. A full “theory”** of weight regulation must consider all signals
The Start of a New “Theory”
A theory is a system of ideas intended to explain something, especially one based on general principles independent of the thing to be explained. Essentially, a theory is a set of ideas that are substantiated by individual hypotheses. Thus, a new theory of weight regulation must consist of several independent ideas that we can test empirically that all add up to a coherent set of ideas.
Let me explicitly set out my theory of weight regulation in a series of clear, concise ideas.
- Body weight is regulated by the net change in the energy going into the system and out of the system (the body).
- The energy going is regulated by the food intake.
- The energy going out is regulated by a complex interaction of varying stimuli.
- The “quality” of the tissues in the body is also regulated by the complex interaction of the same stimuli.
When we boil this theory down we can describe it in a relatively simple set of equations.
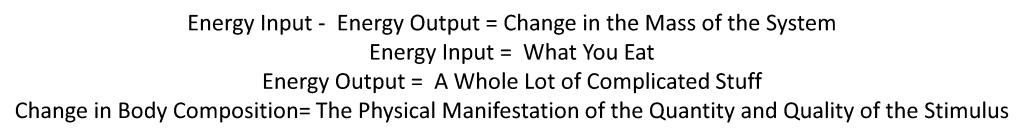
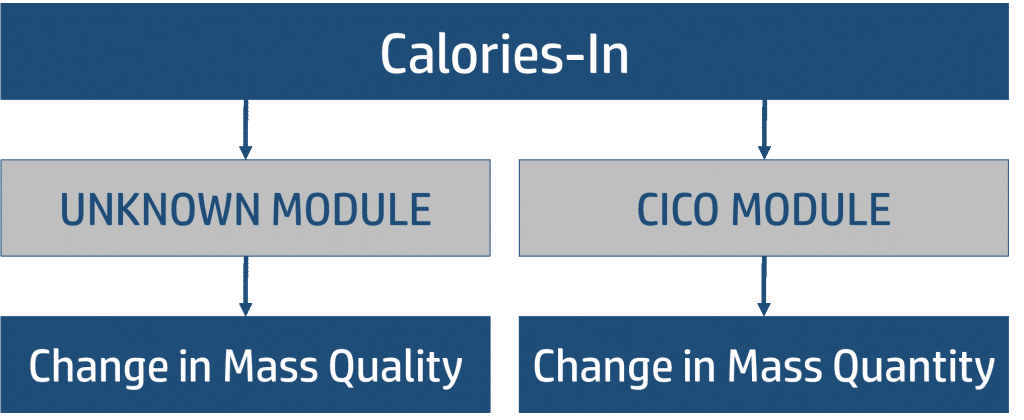
This new “theory” does not necessarily through the baby out with the bathwater. In fact it utilizes current knowledge and organizes them into a hierarchy. It is, in essence, a refinement of ideas into a parsimonious model. It does require us to shift our thinking in some areas. First, we need to separate our vague notion that the weight of the system (i.e. the total) mass reflects the “quality” of the system (i.e. the body composition). So from a heuristic standpoint we can begin to think about our model as stratified from the beginning (this is a crude approach but it begins to separate our thinking, we will bring them back together in the end).
When we distill the concept of CICO into our new theory of weight regulation we allow it to govern the “energy balance” part of the equation. In the roughest sense, we can allow CICO to remain relatively intact and acknowledge that if we wish to simply estimate the change in the mass of the system (i.e. the amount of weight gain or lost) we can approximate it quite closely using CICO as a “module” in our theory.
Let us explore this module a bit more. Within the CICO module we have our input, which is food, and we have our output, which is our energy expenditure. Between the input and the output we have even smaller modules that each contribute to the overall amount of energy that is being expended.
As you notice, we have weighted portions of the module to reflect their relative contribution to the energy output. This needs some explanation. You will notice that we do not have what most people consider the most important factors (age, weight, height). The reason for this is quite simple, those factors all act upstream of our “micromodules” and can be accounted for in the pieces represented (e.g. hormones, NEAT, BMR). We have also selected a few key hormones that represent different aspects of human physiology: neuronal regulation of hunger, basal metabolic rate, and gastric regulation of hunger (ends up having central nervous system effects but you get the idea). You will notice that exercise makes up substantial smaller piece of energy expenditure than non-exercise activity thermogenesis aka NEAT; the amount of physical activity you get just moving around during the day. Environment also plays a fairly important role in energy expenditure; for example, living in cold temperatures can substantially increase energy output. Importantly, you will also notice that the food component makes up the smallest piece of the expenditure. While there are minor differences on energy output based on the thermic effect, the hormonal changes, and the timing of your food choices, the relative contribution to your total expenditure is highly insignificant when compared to the rest of the things that control expenditure. Importantly, all of these are modifiable, meaning you can turn these knobs through your lifestyle.
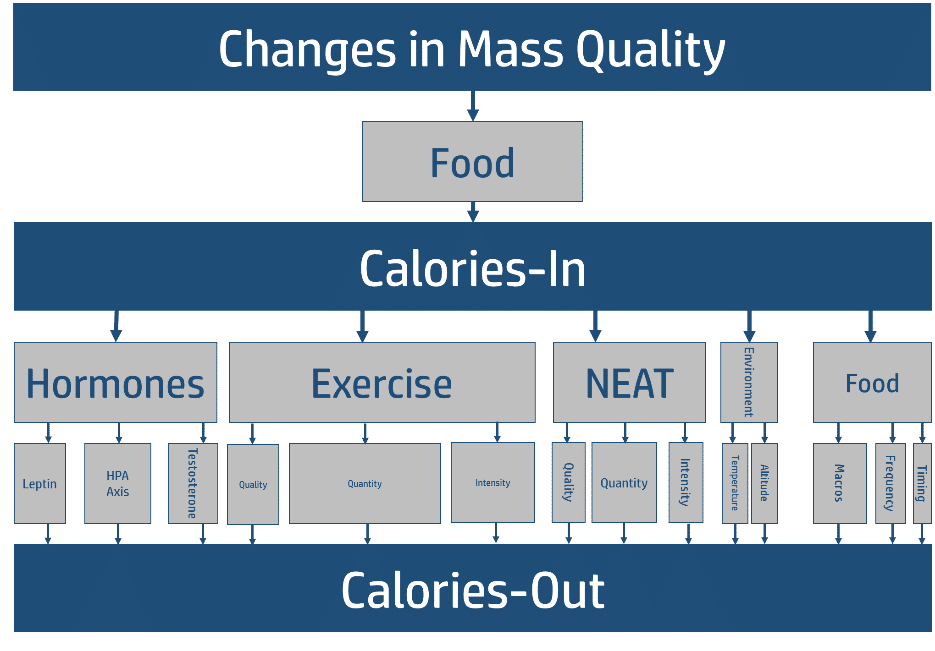
Changes in Quality
Now that we have addressed changes in the quantity of the mass of the system (i.e. the number on the scale) now we need to address the changes in the quality of the mass of the system (i.e. the relative amounts of muscle, fat, bone, and overall metabolic health of these systems and other organs). As you can see in the figure below the overall “modules” in this piece are the same as those in the Change in Mass Quality Modules, they are just weighted a bit different.
The first large difference is the exercise piece. Decades of research have clearly shown that specific modes of training elicit specific physiological adaptations. For example, resistance training elicits a robust hypertrophy response in skeletal muscle while aerobic training elicits more metabolic responses (i.e. increased mitochondria). Secondly, we know that the volume, or quantity, of the work you do is a major driver of physiological adaptation. Thus the quality, quantity, and intensity of the work you do dictates a large portion of the changes in mass quality. We will discuss this in more depth in a future post but for now, this explanation gets us 90% of the way there.
Decoupling Our Ideas
The prevailing idea is that energy balance is at the bottom of all things regarding weight regulation. I find this to be a tad myopic, it neglects the second module of changes in quality of the system. And although the two are inexplicably linked, we can decouple our ideas of Tissue Quality and Tissue Quantity. This actually allows you to make adjustments and adaptations to your body in a much more nimble way than the over simplistic approach about calories-in-calories out. At bottom, it is about calories when it comes to weight. When it comes to tissue quality it is about calories in, and the work being done and the signals driving tissue adaptations.
Applying the framework
Reasoning by analogy is inherently flawed and narrows the scope of our ability to think about a topic; however, in this situation I think an analogy gets us part of the way there. Imagine the body is a mixing board. When using a mixing board a signal of energy comes in and you move knobs and levers to control the volume, pitch, and frequency, of the signal that goes out. The body is similar and you have a lot of knobs that determine the amount of energy that leaves the system and what that energy does to the system while it is in there. The levers and knobs consist of our hormones, our activity levels, our sleep, our type of training, and a lot of other things we probably don’t even know about.
Now we get to the hard part, which knobs are most important, and which ones do we turn to augment our fat loss. The answer? No one has a very good idea of the exact contributions in normally functioning human physiology. However, it is safe to say that at given times we are able to use clues and hints as to which knobs to turn and focus on. For example, if a client comes to you and has had substantial trouble losing weight despite a low calorie diet (~1,200 kcal/day) and substantial exercise (assuming this is true and they aren’t misinforming you) and blood work comes back with a T4 level of 0.6 ug/DL then you know that cutting more calories to around 800 kcals/day is probably not the solution to fat loss.
Based on the current state of knowledge we can use systematic inquiry (essentially guess and check) to fine tune nutrition, training, and lifestyle to adequately address each of the components that dictate changes in weight (quantity) and body composition (quality). People who are solely interested in the number on the scale simply have a math problem, albeit a complex one. In those cases you should focus on the modifiable “knobs” or modules that have the biggest impact on the energy balance equation: Food intake, NEAT, exercise, and hormones; however, the exercise piece is really the least important piece to emphasize for energy balance amongst these.
The people who are interested in changes to the quality of the system present a harder challenge. In addition to the balancing of the energy scale you need to really consider training modalities, hormones, and macros to a much bigger extent. These two things can have a substantial effect on the outcome. For example, if someone wants to lose twenty pounds you can really give them any ratio of macronutrients (example: 10% protein, 70% carbs, 20% fat) you want and any type of training program (buy one of those crappy programs from a facebook ad and give it to a client) and if you have the right caloric deficit and hormones aren’t completely disastrous you can get that scale to move. Conversely, if you have someone who wants to add 10 pounds of lean muscle mass and lose 10 pounds of fat mass (net balance on the scale) that same approach is going to be a disaster.
Conclusion
That was over 4,500 words to essentially say that Weight Regulation ought to really be thought about as two “overlapping magisterial”. Weight Regulation of the human body is best thought of in terms of Quantity (weight) and Quality (types of tissue). Quantity is easily understood and explained by thermodynamics and is, in essence, a math problem. Quality, or body composition, is best thought of as a complex mixture of signals that range from food type to hormones to exercise type, quality, and frequency. While this framework is not simple, it gets us much closer to the truth and allows for more nuanced discussion and a better way forward. The next piece in this series will flesh out the models even further and get down into a little more detail with how we should think about this topic on a “societal and global” scale.
*There are some interesting hypotheses about how the laws of physics may not be homogenous throughout the entire universe, but even if true all experimental evidence indicates that the established laws of thermodynamics hold true here on earth, where this discussion is being had.
**Using the word theory implies a very special meaning. Comments about how gravity is “just a theory” really misses the mark. Don’t be one of those people who assumes a theory is an idea held together tenuously by disparate pieces of data. . . .